Breathing Muscle Weakness in NMD
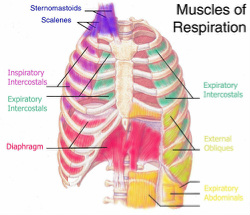
Simply put, in Neuromuscular Disease (NMD), as muscle-wasting progresses, the muscles involved in breathing (diaphragm and intercostal muscles) can weaken. More specifically, the ability of the lungs to expand and take in Oxygen (room air) and exhale the waste product of that air (Carbon Dioxide or CO2) becomes difficult as these processes involve the use of muscles. This causes a gradual increase in Carbon Dioxide levels in the lungs and blood (hypercapnia). The ability to clear lung secretions (mucus) by coughing forcefully becomes impaired as well, putting the individual at risk for developing respiratory infections and mucus plugging (when bronchial secretions accumulate and obstruct airflow). This can lead to respiratory infection and can progress to pneumonia.
Weak breathing muscles cause risk for respiratory failure, the most common cause of death in those living with NMD. Today's advances in medical care makes this complication manageable through the use of respiratory muscle aids (i.e. a Bi-level device such as a BiPAP or portable ventilator and a device often referred to as an insufflator/exsufflator or cough-stimulating device such as the CoughAssist by Philips Respironics).
Understanding How Breathing Complications Develop
When breathing issues begin for an individual living with NMD, they often show up in the form of sleep-disordered breathing, causing the individual to awaken frequently throughout the night, awake with morning headaches that go away after being awake for a few minutes; and this sleep-disordered shallower breathing can cause progressively worsening daytime sleepiness and fatigue.
But how can NMD affect your breathing in the first place? Most progressive breathing problems develop because of one or more of the following reasons.
• The individual has a smaller lung volume where the chest has less room to expand due to respiratory muscle weakness or a recent loss of the ability to walk.
• The individual has respiratory muscle weakness that is causing a weakened cough not powerful enough to clear lung secretions.
• The individual has swallowing problems due to weak throat muscles causing food to go down the wrong way.
• The individual's disease has caused a physical change to the skeletal structure of their body such as scoliosis (a progressive curving of the spine) that has limited the chest cavity size and shape, meaning the lungs can’t grow and/or expand normally.
If you have NMD or a loved one does and you have any questions about breathing muscles being influenced by any of the above, please make it a priority to schedule an appointment for a respiratory evaluation with a Neuromuscular Disease specialist who understands the breathing issues associated with Neuromuscular Disease. These are commonly found at university-based hospital systems.
For more information on breathing issues in NMD, we recommend Muscular Dystrophy Canada's Guide to Respiratory Care for Neuromuscular Disorders. We find it easy to understand and comprehensive in the information it includes.
Note: The following are Neuromuscular diseases that can result in chronic alveolar hypoventilation (under ventilation that can result in elevated Carbon Dioxide, CO2, in the blood).
Myopathies:
Muscular dystrophies:
Dystrophinopathies (Duchenne, Becker)
Limb-girdle
Emery-Dreifuss
Facioscapulohumeral
Congenital
Childhood autosomal recessive
Myotonic dystrophy
Congenital and metabolic myopathies
(such as acid maltase deficiency)
Inflammatory myopathies
(such as polymyositis)
Diseases of the myoneural junction
(such as myasthenia gravis)
Mixed connective tissue disease
Learn more at: http://www.rtmagazine.com/2007/02/respiratory-care-of-the-patient-with-neuromuscular-weakness-the-not-so-new-paradigm/#sthash.pwSxRunZ.H0skLZbj.dpuf.
Simply put, in Neuromuscular Disease (NMD), as muscle-wasting progresses, the muscles involved in breathing (diaphragm and intercostal muscles) can weaken. More specifically, the ability of the lungs to expand and take in Oxygen (room air) and exhale the waste product of that air (Carbon Dioxide or CO2) becomes difficult as these processes involve the use of muscles. This causes a gradual increase in Carbon Dioxide levels in the lungs and blood (hypercapnia). The ability to clear lung secretions (mucus) by coughing forcefully becomes impaired as well, putting the individual at risk for developing respiratory infections and mucus plugging (when bronchial secretions accumulate and obstruct airflow). This can lead to respiratory infection and can progress to pneumonia.
Weak breathing muscles cause risk for respiratory failure, the most common cause of death in those living with NMD. Today's advances in medical care makes this complication manageable through the use of respiratory muscle aids (i.e. a Bi-level device such as a BiPAP or portable ventilator and a device often referred to as an insufflator/exsufflator or cough-stimulating device such as the CoughAssist by Philips Respironics).
Understanding How Breathing Complications Develop
When breathing issues begin for an individual living with NMD, they often show up in the form of sleep-disordered breathing, causing the individual to awaken frequently throughout the night, awake with morning headaches that go away after being awake for a few minutes; and this sleep-disordered shallower breathing can cause progressively worsening daytime sleepiness and fatigue.
But how can NMD affect your breathing in the first place? Most progressive breathing problems develop because of one or more of the following reasons.
• The individual has a smaller lung volume where the chest has less room to expand due to respiratory muscle weakness or a recent loss of the ability to walk.
• The individual has respiratory muscle weakness that is causing a weakened cough not powerful enough to clear lung secretions.
• The individual has swallowing problems due to weak throat muscles causing food to go down the wrong way.
• The individual's disease has caused a physical change to the skeletal structure of their body such as scoliosis (a progressive curving of the spine) that has limited the chest cavity size and shape, meaning the lungs can’t grow and/or expand normally.
If you have NMD or a loved one does and you have any questions about breathing muscles being influenced by any of the above, please make it a priority to schedule an appointment for a respiratory evaluation with a Neuromuscular Disease specialist who understands the breathing issues associated with Neuromuscular Disease. These are commonly found at university-based hospital systems.
For more information on breathing issues in NMD, we recommend Muscular Dystrophy Canada's Guide to Respiratory Care for Neuromuscular Disorders. We find it easy to understand and comprehensive in the information it includes.
Note: The following are Neuromuscular diseases that can result in chronic alveolar hypoventilation (under ventilation that can result in elevated Carbon Dioxide, CO2, in the blood).
Myopathies:
Muscular dystrophies:
Dystrophinopathies (Duchenne, Becker)
Limb-girdle
Emery-Dreifuss
Facioscapulohumeral
Congenital
Childhood autosomal recessive
Myotonic dystrophy
Congenital and metabolic myopathies
(such as acid maltase deficiency)
Inflammatory myopathies
(such as polymyositis)
Diseases of the myoneural junction
(such as myasthenia gravis)
Mixed connective tissue disease
Learn more at: http://www.rtmagazine.com/2007/02/respiratory-care-of-the-patient-with-neuromuscular-weakness-the-not-so-new-paradigm/#sthash.pwSxRunZ.H0skLZbj.dpuf.
