|
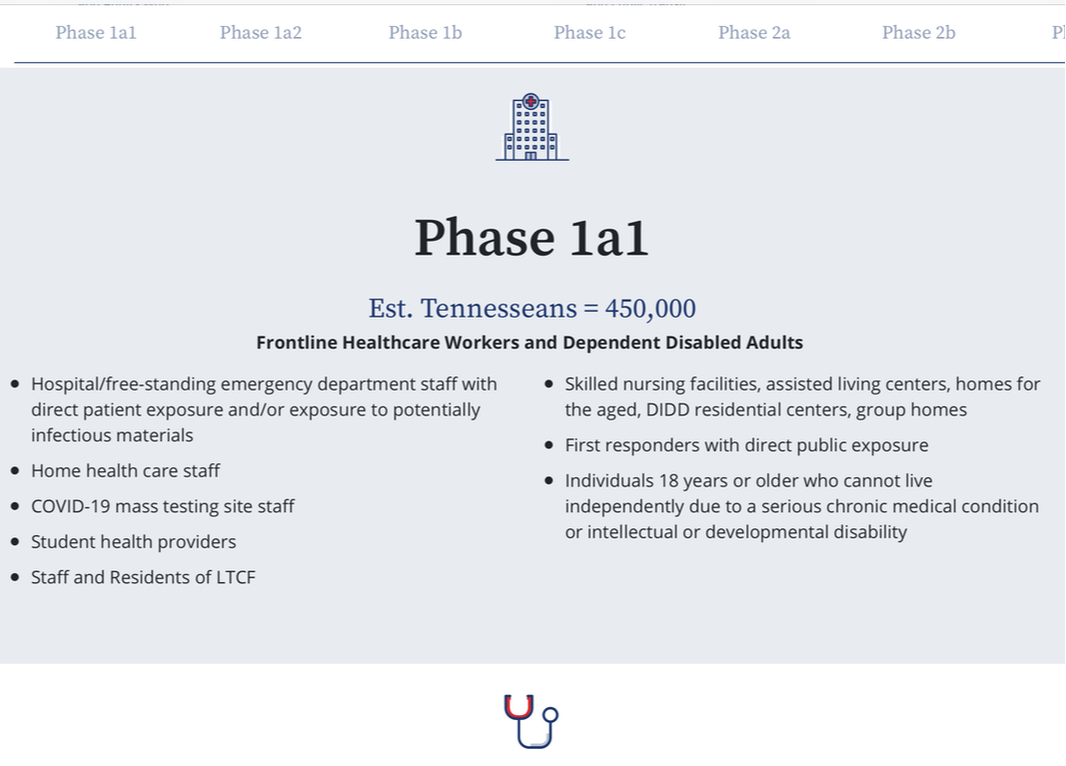
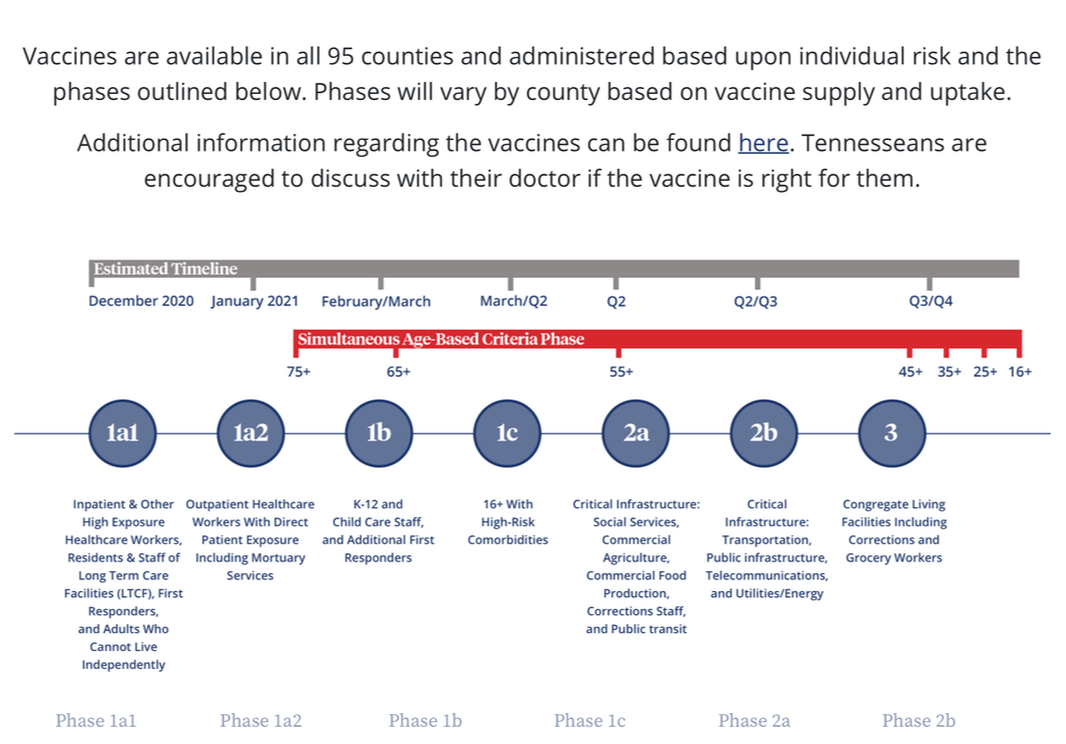
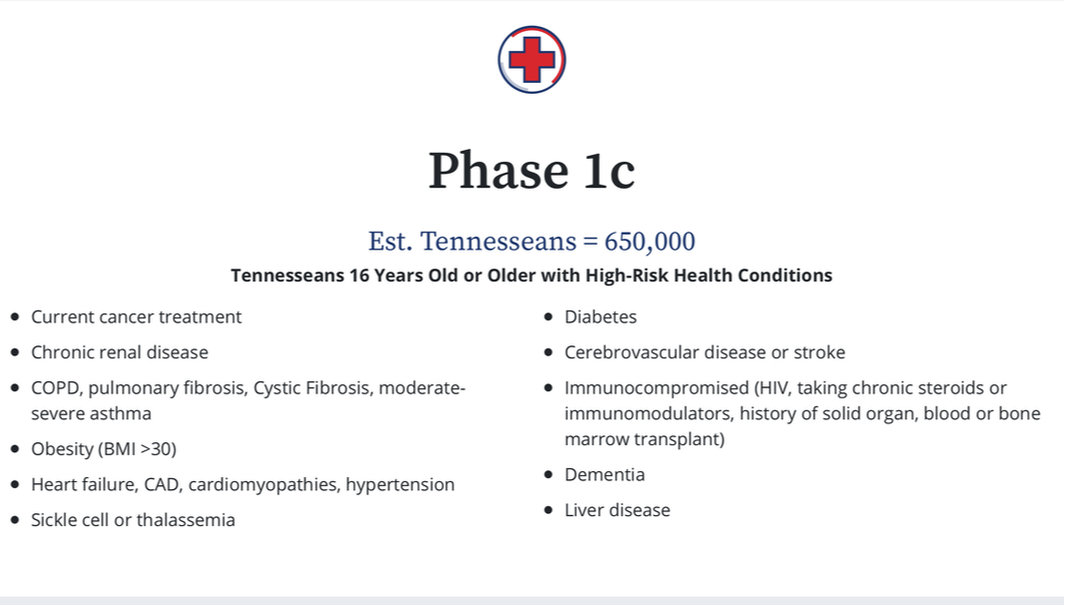
Dear Andrea, I heard you got the COVID-19 vaccination. How were you able to get it, and what if any side effects did you experience? Sincerely, Individual Living with NMD Dear Individual Living with NMD, I got my first dose of the Pfizer COVID-19 vaccination on January 14 through my county's health department in Tennessee, the only way one can obtain the vaccine here at this time, unless you are a resident in a long term care, assisted living, or group home facility. It was not an easy path to navigate, however. My self advocacy process started on December 31, 2020 when I learned my state had updated vaccination priority Phase 1a1 to include "Individuals 18 years or older who cannot live independently due to a serious chronic medical condition or intellectual or developmental disability," the last bullet point in their documentation. This accurately describes my functional status; I could not live independently at this stage. I have help with many tasks by two members of my family. Knowing how things usually go, I felt I was going to have to prove I could not live independently, more so because the vaccinations are given in a drive-through format, and it's not obvious I use a powerchair since I transfer from it into my van's seat. In an effort to get a letter of proof, I emailed my neurology specialist through the patient portal. I requested a letter to explain, based on my diagnosis, that I could not live independently and shared a hyperlink to the state's Phase 1a1 verbiage that references adults who cannot live independently. On the first business day of 2021, I got a response with a letter for use as proof of eligibility. Although it explains my diagnosis, functional status (including noninvasive ventilator dependence), and my need to get a COVID-19 vaccination as soon as possible, it does not reference the state's Phase 1a1 verbiage. I wasn't too concerned though, because another individual had just shared in a Facebook group that her Tennessee county's health department required no proof of inability to live independently. Next, I called my county's health department, knowing they still were not scheduling COVID-19 vaccinations due to lack of inventory. But my goal was to confirm what they required for eligibility under the Phase 1a1 bullet point on "adults unable to live independently." In my mind, I figured I already had that proof in the form of the printed letter and would soon be able to schedule the shot. "Wishful thinking" on my part... The staff member did not know this part of Phase 1a1 existed. I read the verbiage from the state's website and told her where I found it. Then she said she didn't think that was for anyone other than nursing home or group home residents. I explained that not all of us with significant disabilities live in those situations and that I live in my own home with my husband who acts as my primary caregiver. She agreed to check with her supervisor for clarification and asked me to call back the next day. I called back, and she had not gotten an answer from her supervisor. She was awaiting a response from an email the director of the county health department had sent to the Tennessee Department of Health seeking clarification. She asked that I call again the next day and that most likely the answer would be available. I did that, and this time I spoke to another staff member who was unaware of my prior discussions and knew nothing about this aspect of Phase 1a1. I explained everything I had to the previous representative, and she placed me on hold to speak to her supervisor about the email. When she returned, she asked, "Do you work?" I shared that I work a reduced 30-hour per week schedule via an ADA accommodation. That's when she said this portion of Phase 1a1 was for those on social security disability. I explained that not all of us with high risk for severe COVID-19 complications are on SSI or SSDI; some of us work. She continued to ask if I was using Medicaid or any state benefits. I explained that I was not, that my employer provided health insurance for me and that my ability to work or not use state benefits should have nothing to do with my risk level and access to the COVID-19 vaccination. She agreed to check into it this further and said she would call me back. I shared my phone number and waited. The next day, this staff member called and said I was indeed not eligible for the vaccination under Phase 1a1 as it was, "for those who can basically do nothing for themselves." I then asked which phase I could get vaccinated under and explained that Phase 1c, not yet being scheduled for vaccination, showed verbiage for many different co-morbidities but did not list my condition. She assured me that Muscular Dystrophy would be classified under under Phase 1c, and our call ended. I felt defeated at the thought that I would be waiting an estimated two months on Phase 1c. I placed a public post on my personal Facebook page that resulted in individuals involved in advocacy for the disabled commenting and/or private messaging me next step suggestions. One of those suggestions was to reach out to my state representatives (state house and state senate). One state senator in particular was recommended, as he is known to be understanding of disability related concerns. I mentioned this to my oldest sister and learned she had gone to school with him from elementary through high school. She said she would see him in town occasionally and would chat. She suggested I should mention my relation to her in my letter. That Friday night I wrote a letter to that particular state senator and of course referenced my sister knowing him from school. I wrote to him "seeking suggestions about my unique situation with the county health department." I concisely described my understanding of the "dependent adults" aspect of Phase 1a1, shared the state website's verbiage about it along with screen shots from the website, and a hyperlink. I expressed my concern that it seemed I was being excluded on the basis of my ability to work and not use state benefits. I signed the letter with my phone number beneath my name. Early Monday morning, while I was working from home, the senator called and left me a lengthy voicemail explaining he had reached out to individuals at the state level over the weekend and that I did qualify for the COVID-19 vaccination under Phase 1a1. He suggested I call the county health department later that morning, giving them time to get the information from the state department of health to explain this aspect of Phase 1a1 to them. He said I should ask to be scheduled for the vaccine, assuming they had inventory for appointments. A couple of hours later, I called. The recording stated they had no inventory and would not be scheduling COVID-19 vaccination appointments that day. I hung up, but much to my surprise, the director of the county health department called me two hours later. She was up to date on the situation and asked if she could place me on a waitlist when I explained I had hung up after hearing they had no inventory. (Their greeting never referenced a priority waitlist.) I received an email confirmation of my being added to the waitlist a short time after our call. I was ecstatic to simply be on that list! Just when I thought the hurdles were all behind me, two days later, an appointment scheduler at the county health department called and tried to tell me I was NOT eligible. I persisted and explained the process I’d followed up to that point, and that the director herself had added me to the waitlist. That was acceptable to the scheduler, but she asked what I was told to bring as proof. I explained I had not been told proof was even required but that I had a letter my neurology specialist had written. I was warned I would be turned away at the vaccine site if my proof was not sufficient, yet she couldn't tell me herself what proof was required. The appointment was made for 3:15 p.m. that next day. Annoyed and fearing I would be turned away, I picked up the phone and called the health department, asking to speak to the director by name. I reached her voicemail and told her I was really confused. I explained she had personally added me to the waitlist after telling me she'd been told I was eligible under Phase 1a1, but now her staff member who scheduled me threatened that I better have proof or I would be turned away. I explained that I would appreciate a call back, because I didn't want to take off work and go for the vaccination if I was simply going to be turned away and my specialist's letter wasn't adequate proof. While I awaited her call back, I remembered the end of the state senator's voicemail, "You give me a call if you have any other problems with the county health department not allowing you to get your vaccination." I called and was able to reach him. He agreed to call the director to get this confusion cleared up. He also agreed to check with an attorney he'd communicated with at the state department of health when he originally researched this. Moments later, he called back and said the state attorney recommended I take the email string where he and another staffer said I personally met the qualifications for getting the vaccine under Phase 1a1. The senator forwarded that email string to me and asked that I print it and carry it to the appointment for the vaccine the next day. Moments later, my phone rang again, and it was the director of the local health department, returning my call. She explained in not so many words that the scheduler who told me I better bring adequate proof wasn’t trained to understand that she didn’t have to push me like she does those able-bodied folks trying to get around the system by lying about their vaccine eligibility. She was very nice and reassured me that at my appointment the next day, she herself would be registering people at the check in point and that she would not need proof. In fact, she said my portion of Phase 1a1 was the only one that didn't require identification or any other proof (which I found a little strange). That was not actually what happened the next day. My husband drove me there, and right away, when we answered the check in staff member that I was part of the Phase 1a1 provision for adults unable to live independently, we were given a strange look. My husband handed her a stack of emails and said this was the proof of the approval I'd received from the state to get the vaccination. She took the stack of papers and asked us to pull out of the line. I thought, "Here we go! This is where they send us home!" This individual was not the director of the county health department. "Where was she!?" I wondered. Well, she wasn't far away, and thankfully this individual took the stack of papers to her and mentioned my name. We could hear from our van with rolled down windows, "Oh, she's good to go. We've cleared her." From there, it was smooth sailing. We were ushered to the line where I was asked a few questions pertaining to allergic reaction risk, and in about five minutes, the needle was in my arm. I looked away and barely even felt it! It was a split second pinch and was less painful than many annual Influenza vaccinations I've received. You've made it this far, so you must be wondering how my body reacted to the COVID-19 vaccination. My symptoms in the hours after dose one were identical to that of other vaccinations I've received (Influenza and Pneumococcal). My arm was increasingly sore, the more time that passed. Within 26 hours, the soreness was gone. I never ran a fever, but I had a few short episodes of chills followed by hot flashes. I had some mild fatigue, but I experience a degree of fatigue daily, so it would be hard to say whether this was vaccination-related. I also had brief episodes of mild nausea that were intermittent the evening after the vaccination into the following morning. Two days later, I experienced a 3-4 hour period of slightly worse mild nausea. I had to nap through that, but I believe my going too long between meals may have increased the nausea. Obviously, these were minor inconvenience type symptoms that were well worth experiencing in order to work towards developing some immunity to COVID-19. All total, my process to get the first dose of the Pfizer COVID-19 vaccine involved nine phone calls and two emails. It shouldn’t have to be this way, but most of us who have lived with a disability for any period of time know few things come easy in the real world for us, and self advocacy is a must! In closing, if you plan to get a COVID-19 vaccination, I encourage you to research your state's prioritization schedule as soon as it becomes available and keep abreast of any changes to it. Don't be afraid to contact your county and/or state health department for clarification on eligibility. And if you hit a road block so to speak, reach out to your state representatives for their suggestions and assistance. And of course you can count on me to document my Pfizer COVID-19 second dose vaccination experience in this blog. Check back in February for that! All the best, Andrea  Cheryl Lewis with her toy poodle Leo, seated in her power wheelchair Cheryl Lewis with her toy poodle Leo, seated in her power wheelchair Normally my blog post answers a community member's question(s). In this post, I'm taking a departure from that. - Andrea Klein Everyone has had an awful birthday, right? Maybe you had a party with poor turn out or were sick that day. December 10, 2007 was my worst birthday ever and is seared in my memory because my middle sister Cheryl died. Instead of unwrapping gifts or eating cake, I was standing in a hospital hallway hearing, "I'm so sorry; she just passed. She fought hard." It was a day of many tears and shock; my birthday was the last thing on my mind. Cheryl had been hospitalized since the evening of December 1 for a respiratory crisis related to what was then known to us as Limb Girdle Muscular Dystrophy. (Now there are more than 30 identified subtypes of this disease.) In hindsight and with new understanding gained from the books of Dr. John R. Bach, I realized hospital ER and ICU staff hastened Cheryl's death. They failed to check her carbon dioxide level and focused on her low oxygen saturation; that only told part of the story. They ignored her obvious symptoms of carbon dioxide retention or hypercapnia. She had explained she was nodding off and seemed to be losing consciousness for seconds to a few minutes at a time, even while talking or eating. She showed them her newly swollen ankles, an issue that started towards the end of November. She said she had been having hand tremors for months. She also told them she could not breathe while lying flat, but she wasn’t sure if that was anxiety since she physically could not get up from a reclined position unaided. Prior to her ER visit, when her primary care physician was stumped and could only help move her neurology appointment up by a week or two, we searched the MDA USA website. The information about breathing issues was specific to ALS and Duchenne. Knowing she had neither, this was of no help to us as we expected the treatment would be different. I turned to Google and found an article on respiratory acidosis. It covered some of the symptoms she had been experiencing. The hospitalist in the ER agreed to take the article, but he seemed uninterested. In his defense, the article didn't mention Muscular Dystrophy as a potential cause. In the ER, clinicians started Cheryl on supplemental oxygen without mechanical ventilation. It was the catalyst for a firestorm of medical errors. Around 10 p.m., my Mom called to let me know that she had perked up and felt much better. The plan was to observe Cheryl overnight and discharge her with an order for oxygen and the directive to see a pulmonary specialist. That did not happen. Settled in her hospital room, she began to speak to family members in an uncharacteristic way. Then she had a verbal outburst with a clinician who wanted to do an arterial blood gas, (something that should have occurred when she arrived in the ER). Soon after, she went into respiratory arrest. The oxygen she was getting via nasal cannula created more "waste product" of that inhaled air, and this carbon dioxide backed up in her lungs that were too weak to expel it at an efficient rate. She had to be intubated which took multiple, difficult attempts. It was a pediatric tube that finally fit her narrow airway. Up until the tube went in, an ambu bag (manual resuscitator) was used, and an eardrum ruptured and bled. She was quickly taken to ICU, and that was when my Mom called again. Our family rushed to the ICU waiting room where we were sleep deprived, crying, and praying. “Throughout the entire ICU stay, one thing was constant: uncontrolled, high levels of carbon dioxide.”  Cheryl Lewis, seated in her power chair with her dog Leo, next to her Christmas tree in 2006. Cheryl Lewis, seated in her power chair with her dog Leo, next to her Christmas tree in 2006. Over the next few days, Cheryl was in ICU on mechanical ventilation with supplemental oxygen and sedatives. A few days into the stay, she had an emergency tracheotomy after another close call with respiratory arrest and no improvement in her high carbon dioxide level. She developed blood clots in the surgical site and had a bronchoscopy to remove clots from her lungs. She had a suspected allergic reaction to a drug used to reduce retained fluid and then developed pneumonia. A culture was taken from a line placed in her femoral artery and was found to be a severe infection known as sepsis. Next she suffered from lung collapse, first one and then a second lung. Throughout the entire ICU stay, one thing was constant: uncontrolled, high levels of carbon dioxide. It was multiple organ system failure that delivered the final blow to her body. Around 7 a.m. on December 10, she died. It's so painful that we did not recognize incomplete or wrong care was being provided prior to her respiratory crisis and during it. You know what they say about hindsight being 20/20. We were at the mercy of our small town hospital. They didn't know much about Muscular Dystrophy and apparently nothing about the associated respiratory involvement. That's what I want to stress to you. The burden, as if you needed anymore, is on you and your loved ones to understand how neuromuscular disease can weaken the muscles we use to breathe and cough; what makes this better; and what can worsen it like unventilated supplemental oxygen. (Learn more about the dangers of unventilated supplemental oxygen at https://breathewithmd.org/oxygen-caution.html.) The less you know about respiratory muscle weakness, the higher the risk for poor outcomes, unless the clinicians you see have experience with neuromuscular pulmonology. Some are blessed to receive amazing medical care by clinicians who do in fact understand breathing/respiratory muscle weakness. However, throughout the years, I’ve come to understand that's uncommon, particularly in rural US communities.
Awareness has increased in the 13 years since Cheryl’s death, in part due to my commitment to share her story and educate my peers. Some nonprofits for specific neuromuscular conditions are including breathing weakness information on their websites, and the quality and detail of this varies. The bottom line is that death from respiratory failure is preventable when proactive measures are taken and continued appropriate care is received. I frequently meet families through Breathe with MD, Inc. that are on the verge of or living through a respiratory crisis like Cheryl’s. It takes me back to those difficult days with Cheryl's hospitalization and saddens me that with all of the advances we've made in research and treatment, this is still occurring. That is why Cheryl’s story must continue to be told. Her life was cut short at age 38 because the medical community failed her. It’s failed many others like her, young and old, before her death and after it. Her death on my birthday devastated my family, but we rejoice that some good has come from it. Her death led me to create the mission and programs of Breathe with MD, Inc. In memory of Cheryl today and to make this my "best birthday ever," I encourage you to get involved with my 501(c)(3) nonprofit public charity. Below are some ways you can do that.
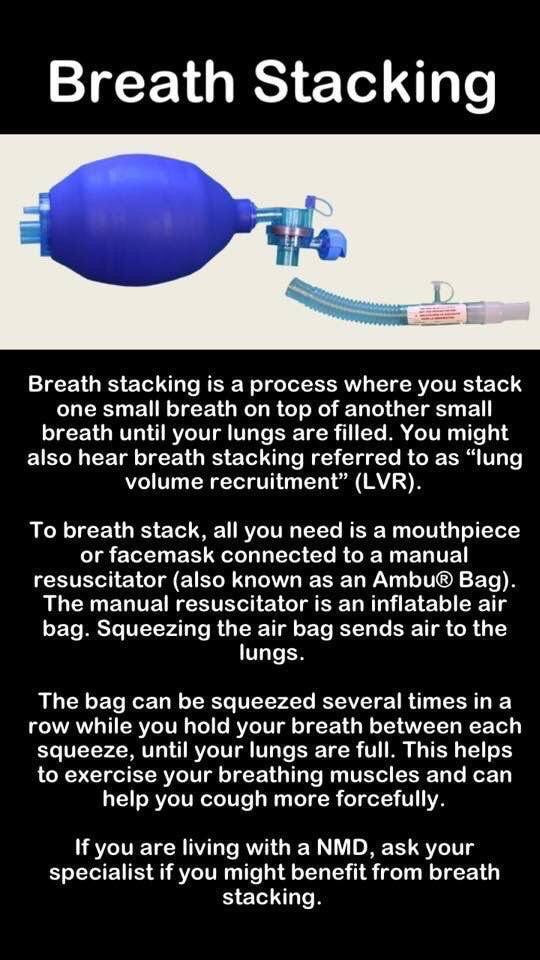
 Grab your favorite beverage and get comfortable! In this lengthy blog post, I'm covering the 10 most frequently asked questions I'm asked by individuals living with a neuromuscular disease (NMD) and/or their loved ones. This blog is jam-packed with videos and links to resources for additional information. As always, don't use this blog post as a substitute for medical care. Seek medical advice about breathing muscle weakness in NMD from a licensed clinician who specializes in the breathing issues of those with NMD. Question 1: Could I be having problems with my breathing? I've gotten several variations of this question, often with a variety of symptoms being shared. A common theme I see is that many adults struggle to accept that their breathing might be affected by their NMD and hope it will just get better on its own or that they are imagining the issue. I get it; it's scary to think about something so critical as our breathing being affected. However, my advice is always the same: If you even THINK you might have a problem with your breathing, or if you haven't had an evaluation of your breathing by a clinician who specializes in the breathing issues of those with NMD, DON'T DELAY seeing a specialist. It should be one of the first things you do after you are diagnosed with a NMD, and it should be followed as frequently as your clinician recommends (usually at least annually). Don't know where to find a clinician? University-based hospitals that include a neuromuscular clinic typically have a pulmonary specialist, neurologist, and/or physiatrist (doctor of physical medicine and rehabilitation, PM&R) who understand breathing muscle weakness in NMD. You can also ask you peers, particularly those with NMD in your area. If you are new to the concepts of breathing muscle weakness, Muscular Dystrophy Canada has published an easy-to-understand, comprehensive, "Guide to Respiratory Care for Neuromuscular Disorders." You can find it at muscle.ca/wp-content/uploads/2019/09/RC13guide-EN.pdf. You can also find a lot of information on the Breathe with MD, Inc. website. Question 2: How can supplemental oxygen be dangerous? Unventilated supplemental oxygen led to my sister Cheryl's death and is why the nonprofit organization Breathe with MD, Inc. exists. Simply put, if you have weakened breathing muscles and low Oxygen saturation, using supplemental oxygen via a nasal cannula while not on mechanical ventilation can make things worse, particularly if you are unable to effectively exhale the waste product of the air we breathe: Carbon Dioxide (CO2). The problem for those with weakened breathing muscles is difficulty moving air into and out of our lungs, a process called ventilation. When we don't ventilate our lungs effectively, it can lead to an imbalance in the level of Oxygen and Carbon Dioxide in our lungs and blood. Use of supplemental oxygen does not improve ventilation and can, in some cases, turn off the respiratory center in the brainstem that tells us to breathe on our own. What we need instead is bi-level mechanical ventilation. I encourage you to watch the short video below. You can get even more detailed information, including links to medical articles to share with your clinician, at breathewithmd.org/oxygen-caution.html. Question 3: Why is CPAP bad for me? CPAP is not recommended for those with breathing muscle weakness, as it offers one continuous positive pressure that is inhaled and exhaled against. When you have weak breathing muscles, exhaling against pressure can be tiring, difficult, and make you feel worse. Instead, you need bi-level ventilation (sometimes referred to as "BiPAP" or a portable ventilator), as these devices offer two different positive pressures. A higher pressure is used for inhalation (IPAP), and a much lower or no pressure is used to exhale against (EPAP). Watch this short video that explains the difference in more detail. Question 4: What is CoughAssist, and why is it recommended? The CoughAssist is a respiratory device sometimes referred to as an "insufflator/exsufflator." Those are big words that mean it helps to make a weak and/or ineffective cough stronger and more productive at removing secretions or mucus from the airways. Learn more in this short animation below. Be sure to ask your NMD care team to determine your peak cough flow (PCF), the velocity of air being expelled from the lungs after a cough maneuver. This measurement can determine whether or not you need assistance with coughing. The CoughAssist can also be used to stretch the breathing muscles much like you would stretch other tightened muscles. I use CoughAssist multiple times a day when well and as often as I need to cough when I'm sick. It's kept me from developing pneumonia or being hospitalized. You can read more about my experience with the CoughAssist in a past blog post at breathewithmd.org/ask-andrea/the-device-you-love-to-hate. To learn the specifics on how to use CoughAssist, check out the manufacturer's documentation at https://www.usa.philips.com/healthcare/product/HC0066000/coughassist-t70-mechanical-insufflator-exsufflator#documents. And lastly, review the benefits of using CoughAssist by watching this short animation.  Question 5: How do I know if my ventilation settings need to be increased? Reach out to your respiratory care team to open a dialogue about why you might need to increase or change your device settings. Speaking from my personal experience, I knew my settings needed to be changed when I didn't feel like I was getting a large enough breath from my ventilation while lying down. Another time, I was experiencing some of the symptoms I had before I began using assisted ventilation such as excessive daytime sleepiness, fatigue, and needing 10-12 hours of sleep to feel rested. Sometimes an overnight, at-home "oximetry study" is useful to measure and record your Oxygen and/or Carbon Dioxide levels during sleep. Think of it as a home sleep study with less equipment and easy enough for you or a caregiver to set up. Recording pulse oximetry and capnography can guide the decision making process for ventilation settings changes. Ask your NMD care team more about this option. Question 6: How can I adjust to using noninvasive ventilation (NIV) at night? This is a common question of "NIV newbies." I was an unusual case; I took to NIV right away. Many find that starting to use NIV an hour or two during the evening while relaxing, reading, watching TV, or playing a video game is a good way to get comfortable with it before trying to sleep at night with it on. Others find they simply cannot adjust to their current mask system and need to try something else. Mask preference is an individual choice; I love nasal pillows and have no issues using them at high pressures. Some hate them and prefer nasal, oronasal or full face masks. Do not hesitate to call your respiratory equipment provider to ask to try different masks and to share any problems, concerns, or questions you may have about the new equipment. Asking your peers is a great way to find out what masks might work best for you. A good way to reach peers is in the Breathe with MD Support Group. Learn a little about what makes it special in this short animation, and if you're not already a member, consider joining today. While I'm sharing about the support group, let's move onto another question about it. Question 7: Why can't my physician, respiratory therapist, or other care provider join the support group? The questioner usually explains they want to share knowledge found in the support group with a clinician, usually one that is located outside of the US. While I don't doubt that a clinician could learn from us, the last thing most group members want is for clinicians with different view points to debate a "best practice" for management and/or intervention. Further, while you may be comfortable with your own physician or respiratory therapist (RT) being a member of the group, understand that others might not want their personal health challenges being read, commented on, or even chronicled for informal research by those clinicians. We make no exceptions to this rule; medical professionals are not allowed to join the Breathe with MD Support Group, unless they personally have a NMD or a loved one does (which is the case for a small number of members). As an alternative, I suggest that you invite your clinician(s) to visit our website https://breathewithmd.org/index.html, our public Facebook page, or find us on Instagram, Twitter, and/or YouTube. I personally put a lot of effort into sharing educational materials on our social media platforms, and our website includes a lot of medical articles that can be viewed and/or printed. Question 8: Why can't I share posts from the support group? Like all private groups on Facebook, it is not possible to share a post from within the Breathe with MD Support Group. That is part of the privacy enabled with the group. You can copy any website links or details about resources, and then paste them into a new post on your own Facebook wall or within another group. Question 9: Does Breathe with MD, Inc. purchase respiratory equipment for individuals with muscle disease? At this time, our small US registered 501(c)(3) nonprofit does not provide any financial support or durable medical equipment for individuals with NMD. You can learn more about our mission and programs at breathewithmd.org/missionandprograms.html. Question 10: Is there an exercise I can do to make my breathing muscles stronger? Unfortunately, with diseased muscle tissue, we don't have the benefit of making it stronger like with healthy muscle tissue. Instead, we can stretch our chest wall muscles so that they may be less restrictive to our rib cage and lung expansion, over time allowing us to fill our lungs with more air. Talk to your NMD care team about lung volume recruitment or breath-stacking. Additionally, you may recall that earlier in this blog post I mentioned use of CoughAssist can stretch the breathing muscles. Well, that's it; I've covered the 10 questions I am most frequently asked by individuals in the NMD community. As always, seek the advice of a licensed clinician for any questions or concerns you have about your respiratory health. The advice I share here is solely based on patient perspective.
Wishing you all the best, Andrea  Dear Andrea, My doctor told me I need to use the CoughAssist. I HATE it. I heard you love it, and I cannot figure that out! What can I do to make myself like it, and why do you feel the way you do about it? Sincerely, CoughAssist Hater Dear "Hater," You are not alone. Many people cannot stand the CoughAssist, and I feel like it's a "missed opportunity" so to speak in our community of NMDers. I also believe the lack of use of this device is often at least part of the path to worsening respiratory health. Having said all of that, I credit the CoughAssist T70 with saving my life. You read that correctly; I know that not only has this device kept me out of the hospital during what were some of the worst respiratory infections of my life, but CoughAssist saved my life one morning. It was October of 2016, and I knew I was not well. I didn't have much more than a mild cough at that point though, and I was using an OTC mucus thinner with expectorant. I awoke during the wee morning hours, threw off my noninvasive ventilation mask, turned off my Trilogy ventilator, and raced down the hall to the CoughAssist on an adjacent bathroom's counter. I was mid "coughing fit," and I felt as though I was slowly choking for air. My husband wasn't far behind me. I used CoughAssist as I always had, but I could tell that mucus was stuck at the back of my throat and would not dislodge. I was starting to run out of air. My lips were beginning to get a slight blue twinge. My fingers shook as I changed the values of the insufflation and exsufflation pressures, and my face was as white as a blank sheet of paper. After a couple of repetitions at the even higher pressures, up the mucus came! It was larger than anything I had ever coughed up, so much so I gagged and quickly "lost my cookies," if you know what I mean. My husband and I both looked at each other like, "What on earth is that!?" as it sat in the sink basin, too large to be easily rinsed down the drain. It literally looked like a small fetus or some sort of alien (maybe that description is TMI), but after consulting my pulmonologist, I learned I had removed a small mucus plug! What would I have done if I had not had my CoughAssist to clear my airway of this blocking mucus?! I really don't want to consider that, because I think calling 911 would have been our only option. I don't know that ambulances come equipped with airway suction. And I highly doubt EMTs know what a CoughAssist is or that those of us living with neuromuscular disease use them. My October 2016 mucus plug experience is just one of many examples of how this important piece of respiratory equipment became a life-saver for me. So, after all of those words, I'm answering your question as to how I could love it so much with the fact that I'm still here to answer your question...because of the CoughAssist. In addition to the life-saving, hospitalization preventing aspect of this device, I came to realize more than a year into my daily use of it, that it had another amazing benefit: it stretched my chest wall muscles and allowed me to take deeper breaths while off my assisted ventilation used during sleep. I don't know about you, but anything that helps me take deeper breaths and feel less like I need help breathing is a winner. As for how you can grow to like it more, the only way is to jump on in! "The water is fine," as they say. You must prioritize it like a daily habit as important as brushing your teeth. Come up with a reward for yourself that you earn after using it X number of times per day (maybe a favorite desert or candy). After you've done this for a week, reward yourself again (maybe a new album download or video game). Make it a full month of daily use of CoughAssist? Reward yourself again! Another way you can make it become a tolerable new habit is to devote a cart or special space to it. In 2017, I devoted a special space to all of my "ancillary" respiratory equipment like the CoughAssist, suction machine, nebulizer, and all of the supplies. I called it my "respiratory desk" and recently upgraded that to a wall-mounted desk and two separate drawer units that better organize it all. I followed a decorative theme to match the room my respiratory desk is located in. It includes special sea shells and decor that reminds me of enjoyable trips to the beach. Whatever it takes to motivate yourself to use the CoughAssist, I urge you to consider doing it! It didn't happen overnight, but through daily use of the CoughAssist for a little more than a year, I saw an improvement in my forced vital capacity (FVC), the measure of the strongest amount of air you can forcefully exhale from your lungs after inhaling your largest breath. I and my then pulmonologist attributed that gain to my CoughAssist usage. It and my nightly noninvasive ventilation was loosening up my tightened chest wall muscles, and making my lungs less stiff and able to hold a larger amount of air. We know from experts in the NMD field that over time, our respiratory (breathing) muscles in our abdomen and between our ribs can become contracted and stiffen just like those at the bend of our elbow, knee, etc. Stretching these out is necessary for maintaining and/or stabilizing our respiratory health. The CoughAssist is our opportunity to implement this as a form of breathing muscle exercise into our NMD care. If you would like to learn more about my love of CoughAssist, just reach out to me at [email protected] and ask for a link to my February 2020 CoughAssist webinar. I promise I'm not a sales person for the CoughAssist, but I can definitely "sell you" on why you need to be using one every single day. Wishing you Happy "Cough Assistance," Andrea  Dear Andrea, I noticed you said in the Breathe with MD Support Group you have never been hospitalized for a respiratory infection. I’ve been in and out too many times to count. Do you have tips you wouldn’t mind sharing for staying well? Sincerely, Trying to Stay Well Dear Trying, I’ve kept several things in my "wellness toolkit" over the last few years that I suspect may be why I’ve avoided hospitalization for respiratory infections. I have had a few respiratory infections, but each has been manageable at home. Always check with your Neuromuscular Disease (NMD) care team for their suggestions on staying well. Many of us have worked with our medical teams to put into place a protocol to attack illnesses as soon as they start. If ever in doubt about whether you're developing a respiratory infection, seek medical care promptly. It's better to be told you have no infection or caught it early than to delay necessary care that could land you in urgent care or the hospital. My seven tips are as follows: 1. Vaccinate! Get an Influenza vaccination in October and stay current on the pneumonia shot your physician orders. Influenza, also known as “seasonal flu.” is a respiratory virus that can have life-threatening effects on those who have NMD. Often it’s not the flu itself that’s deadly but complications like secondary bacterial infections that develop (i.e. pneumonia and/or sepsis). A flu shot isn’t perfect; some who are vaccinated will still get the virus. However, studies have shown that those who were vaccinated had illness that was shorter in duration and less severe, meaning less likelihood for complications to arise. If you poll your adult friends in the NMD community in the US, the majority of us answer with a resounding “YES” that we get a flu shot each and every year. If you haven't gotten yours yet, it isn't too late to do so; but it takes approximately two weeks to build immunity against the Influenza strains included. There are different pneumonia vaccinations, so it’s important to check with your NMD care team to learn whether or not the one you’ve received in the past requires a “booster." And if you've never had a pneumonia shot, most NMD care teams will recommend a pneumonia vaccine, as research supports it can protect you from some types of pneumonia. 2. Avoid / “Hibernate” - When I know that illnesses such as Influenza or stomach viruses are circulating in my workplace and/or the community as a whole, I go into "avoidance mode." I will not go near anyone I know has been ill or has had a family member that was recently ill. I will also avoid touching surfaces in common areas with my fingertips or a grip of my hand like the work restroom door, break room drawer pulls, etc. If I must touch a surface like an automatic door opener, I will use my elbow or knuckles, not my fingertips. For other surfaces, I hold a paper towel or tissue as a barrier between my skin and the surface. If I have no choice but to touch a “community surface,” I wash my hands afterwards or use alcohol hand sanitizer. If these things make me a "germaphobe," that's fine with me. I also will not go to stores or any place other than my place of work during times of peak illness in the community. Staying home while people are out likely spreading illness is another form of defense I like to call "hibernation." I realize this is unrealistic for many of us, however. 3. Stay warm and dry when outside - One of my respiratory infections in the past began not long after I had been forced to stand outside after a fire alarm sounded at my place of work. It was raining lightly, and I got wet and chilled. Within a couple of days, I was sick with an upper respiratory infection that went deeper into my chest. I watch weather forecasts closely and ensure that I’m prepared to stay warm and dry year round, even if caught in an unexpected situation like a fire drill. 4. Get extra sleep, including naps - During times of the year when respiratory illnesses are circulating, I try to get as much sleep as possible, even if that means taking a short afternoon or early evening nap. I always use my assisted ventilation during naps. When I experience that drained, “coming down with something” feeling, getting extra sleep will kick those feelings aside and boost my immunity enough to fight the infection off or make it clear up faster. 5. Gargle at the first sign of sore throat - I know not everyone can gargle liquids in their throat or tilt their head back in the process of doing so. I believe that Listerine brand mouthwash (Cool Mint and similar) has an amazing ability to kill germs that live in the back of the throat. It also works well to break down and remove mucus in the back of the throat. When I feel symptoms of a sore, scratchy throat from sinus drainage or some unknown cause, gargling Listerine three or more times that day will clear up the pain and prevent escalation to a throat or tonsil infection. If an infection like that overcomes my body, I find that frequent gargling of warm salt water specifically with coarse grains of salt alternated with gargling Listerine multiple times a day resolves the illness faster. 6. Use a Nebulizer - I have a small Pari Vios nebulizer compressor and a prescription for Levalbuterol solution but have found that unless I’m already sick with a condition that involves wheezing, "nebulizing" plain saline is sufficient. For me, saline alone begins to break up mucus before I use CoughAssist. Many of my peers prefer one nebulizer medication over another, so ask others what they use and why. Your NMD care team should also have recommendations. Note: If you’re using a metered dose inhaler as a substitute for a nebulizer, you’re likely getting little to no benefit of the inhaled medication, even if you are using a spacer to take multiple "puffs." When you have weakened breathing muscles, a nebulizer helps to consistently aerosolize extremely fine particles of the liquid that can be forced into the airways deeper and more efficiently. 7. Use CoughAssist consistently and multiple times a day, especially when mucus changes in type or color - I use my Respironics CoughAssist T70 no less than twice a day when well but often use it three or four times daily. When I notice my mucus changes color or thickness (eww! TMI!), I increase daily usage of CoughAssist to ensure I get this up and out of my airways as quickly as possible. The longer it stays in my airways, the greater the risk of developing a bacterial infection. That concludes my list of tips. I realize everyone is different, and what works for me might not for you. You also might not have access or the ability to do some of what I do. Either way, perhaps even one of these tips offers you an option you might not have considered as a means to staying well. Best wishes for a healthy year, Andrea Dear Andrea, Do I really need to keep this expensive ventilator? My friend has a BiPAP that costs her so much less. Should I just ask to switch to that? Sincerely, "Cash-strapped" ventilator user  Dear "Cash-strapped" ventilator user, One of the most frequent topics of discussion in our Facebook based Breathe with MD Support Group is "Should I use the ventilator prescribed or switch to a cheaper BiPAP for noninvasive ventilation? My monthly payments to the DME are too expensive." This is a tough question to answer. It should be addressed with your NMD respiratory care team. One place to start that conversation is to ask what specifically about the ventilator is necessary for your respiratory care that is not offered on a less pricey bi-level device (a BiPAP). For example, are you using the ventilator, because it offers the option to enable more than one prescription such as one for day use and another for nighttime use? Are you maybe using the ventilator because you're on a mode of volume-based support or a combination of pressure and volume support? Or, are you using active circuit ventilation on the ventilator with the EPAP (Expiratory Positive Airway Pressure) as zero? If so, switching to a basic bi-level device such as a BiPAP is not going to be a solution for you, as a BiPAP won't offer these options. Below is a listing that compares the two devices and may help you to understand why one device might be more suited to your situation versus the other. Bi-level/BiPAPs offer:
Wishing you all the best, Andrea |
AuthorAndrea is the Founder & President of Breathe with MD, Inc. and served as Ms. Wheelchair Tennessee 2017. Her blog posts are based on experience living with a Neuromuscular Disease. The blogs are not to be used as a substitute for medical care. Always seek medical advice and care from a licensed medical professional. Archives
June 2023
Categories |
Breathe with MD, Inc. is a U.S. registered 501(c)(3) nonprofit organization. Donations are tax deductible to the extent allowable by law.
Note: This website should not be used as a substitute for medical care. For medical care or advice, please seek the care of a clinician who specializes in the breathing issues of those with Neuromuscular Disease (NMD).
Web Hosting by Hostgator
Note: This website should not be used as a substitute for medical care. For medical care or advice, please seek the care of a clinician who specializes in the breathing issues of those with Neuromuscular Disease (NMD).
Web Hosting by Hostgator




 RSS Feed
RSS Feed