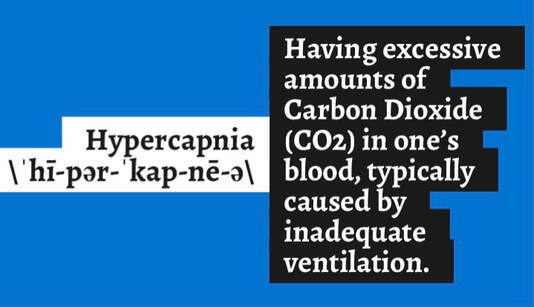
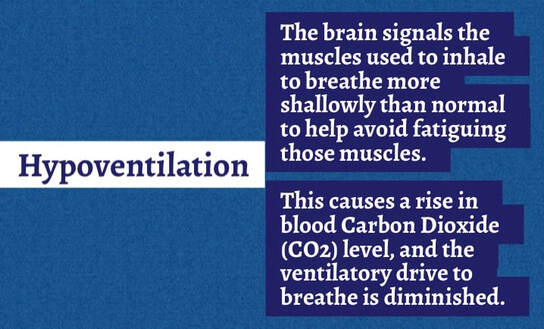
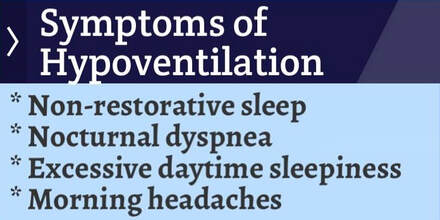
 I think everyone in the United States has heard the term, “being frank.” I am "being frank" because I care about those living with Neuromuscular Disease (NMD) and want to help them prevent a respiratory crisis, something my family experienced in the lead-up to my middle sister Cheryl's death. While I am not a medical professional, I am on the receiving end of all e-mails and social media private/direct messages for Breathe with MD, Inc. I have also received dozens of messages to my own private accounts over the years from individuals living with an NMD who are seeking advice about breathing concerns. Nearly all of these communications have commonalities. One of those is the reluctance of adults with an NMD to prioritize pulmonary care, and it seems to be worse among those with slowly progressive forms of NMD, those that were diagnosed later in life, and those that are extremely busy making a difference in life. There are many reasons why an individual might not prioritize something so serious as their breathing. Sometimes a past medical trauma makes individuals with an NMD fearful or distrustful of medical professionals and their recommendations. Some are simply sick of going to medical appointments and do not believe they can handle another doctor or type of care. Others are fearful of the equipment such as insufflation/exsufflation/mechanically assisted cough (MAC), commonly marketed as Respironics CoughAssist and/or mechanical ventilation due to their lack of understanding or a pre-conceived, incorrect notion. Some wrongfully believe that starting these interventions will make them more dependent upon them over time or become worse simply because they used the respiratory device. Others believe they are so near death that the prescribed interventions will diminish the quality of their remaining life. Still, others have seemingly impossible barriers to accessing a clinician that can provide what is needed where they reside. This deeply saddens me because those of us who have made pulmonary care and interventions for breathing muscle weakness a priority have found that even if the initiation of these devices was a huge challenge, once we got through the adjustment phase, these devices improved our quality of life. Many of us wish we had begun use of the equipment years earlier and regret the delay to start. I personally know individuals with an NMD who have been using mechanical ventilation for 20-30 years, noninvasively with up to 24/7 continuous ventilation via mask and mouthpiece interfaces and invasively with a tracheostomy tube. Needing to start mechanical ventilation is NOT an indication that one's life is near the end, if they are living with an NMD. I can share countless stories to inform you of individuals with an NMD who did not use mechanical ventilation or even get a pulmonary evaluation who suffered from a reduced quality of life or even died. One individual that comes to mind was not using prescribed mechanical ventilation and died in their sleep due to months of unresolved and ever-increasing carbon dioxide (CO2) retention and its escalation to CO2 narcosis and then coma. Another became ill from a cold that quickly progressed to a chest infection, then pneumonia, and was hospitalized, intubated, failed numerous attempts for extubation to noninvasive ventilation and MAC, and nearly died during the ordeal. It took knowledgeable family members advocating and preventing the use of contraindicated interventions (i.e CPAP and unventilated supplemental oxygen). Thankfully, this individual lived to share their story. Still another individual with an NMD had a fall that resulted in a broken bone requiring orthopedic surgery. Their recovery nearly caused their death due to a lack of mechanical ventilation and pain medications suppressing their already reduced ventilatory drive, worsening their NMD-related hypoventilation (under breathing). Getting started on mechanical ventilation can be a challenge when healthy, so waiting until one is recovering from a medical procedure isn't the best or easiest time to do this. All of these individuals and/or their families that I have shared about would tell you NOT to do as they did and to make pulmonary care and the appropriate interventions a priority to prevent poor outcomes. Over the years I have come to know adults that are avoiding the tried and true interventions for breathing muscle weakness and are using what I will refer to as "alternative forms of care." These are attractive because they may be more convenient and/or clinicians that are unfamiliar with breathing muscle weakness and the appropriate interventions are prescribing or supporting the use of them. One common alternative is inhaling nebulized medications that are said to open up airways and help with breathing. There is no research to support use of nebulized medications only for weakened breathing muscles, as nebulized medications are not a substitute for mechanical ventilation and are used for obstructive airway conditions (i.e. asthma and COPD) or during illnesses such as a bronchial infection. Breathing muscle weakness is a restrictive condition and is treated differently. Another "wishful thinking" alternative is muscle training devices whose marketing claims to strengthen breathing muscles. While these devices may provide limited help in stretching weakened and/or contracted breathing muscles, they cannot bring back lost muscle strength that has left as a result of neuromuscular breathing weakness. The bottom line is that these alternatives don't assist us in ventilating (moving air into and out of) our lungs during sleep, and that is what we need help with when a Neuromuscular Disease has led to hypoventilation and/or hypercapnia. In contrast, some of the inter-related benefits of using mechanical ventilation when one needs it are:
Some of the benefits of using insufflation/exsufflation/mechanically assisted cough (MAC) i.e. CoughAssist are:
Please know that the organization I founded, Breathe with MD, Inc., is here to support you through its mission and programs. The Breathe with MD Support Group on Facebook has over 1,700 members, and the respiratory peer mentoring program for adults living with an NMD are excellent ways to get support to make pulmonary health a priority. Many are struggling to accept the gravity of respiratory muscle weakness, but your peers get it and will have suggestions for you. Do NOT give up; you are NOT alone; there are solutions to every challenge you may be experiencing or think you will experience! Wishing you all of the best, Andrea Comments are closed.
|
AuthorAndrea is the Founder & President of Breathe with MD, Inc. and served as Ms. Wheelchair Tennessee 2017. Her blog posts are based on experience living with a Neuromuscular Disease. The blogs are not to be used as a substitute for medical care. Always seek medical advice and care from a licensed medical professional. Archives
June 2023
Categories |
Breathe with MD, Inc. is a U.S. registered 501(c)(3) nonprofit organization. Donations are tax deductible to the extent allowable by law.
Note: This website should not be used as a substitute for medical care. For medical care or advice, please seek the care of a clinician who specializes in the breathing issues of those with Neuromuscular Disease (NMD).
Web Hosting by Hostgator
Note: This website should not be used as a substitute for medical care. For medical care or advice, please seek the care of a clinician who specializes in the breathing issues of those with Neuromuscular Disease (NMD).
Web Hosting by Hostgator

 RSS Feed
RSS Feed