|
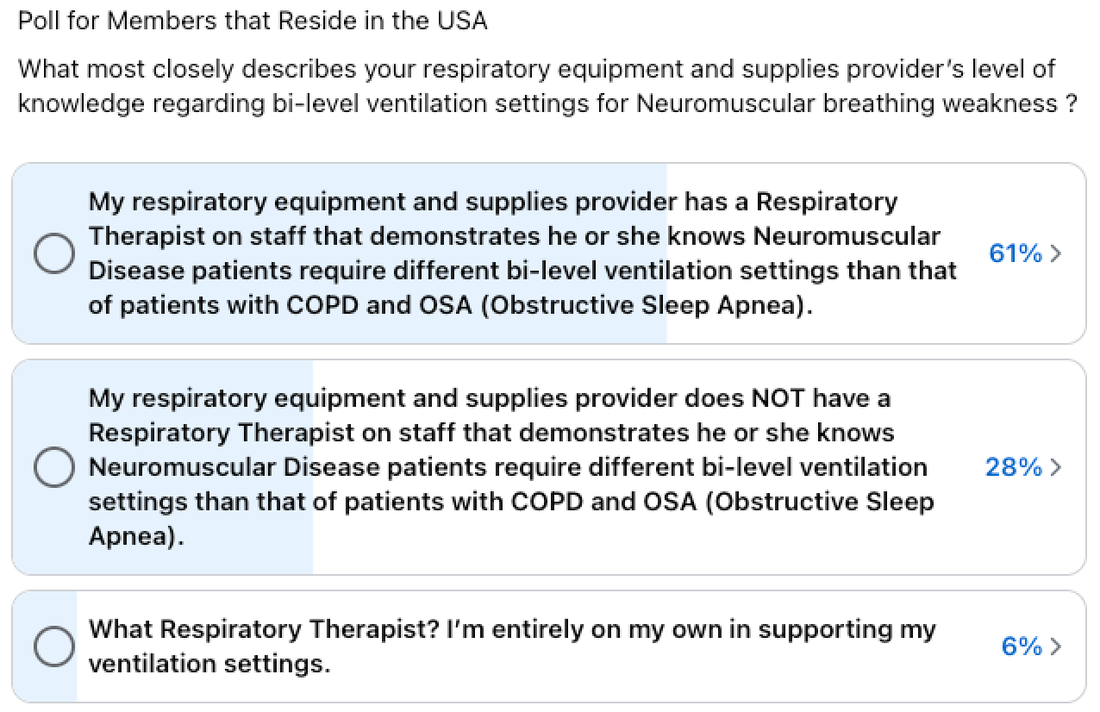
By Andrea Klein Founder & President, Breathe with MD, Inc. "What happened next was unexpected, frightening, and infuriating."  As a user of noninvasive ventilation for nearly 10 years, I used the same brand and model portable ventilator for more than eight of those years. I never anticipated the type of challenges and degree of frustration that I would experience transitioning from that ventilator to one made by a different manufacturer. The process included surprises, delays, and finally…lessons learned. I’m summarizing seven of those here. 1. The prescriber (MD, NP, PA, etc.) can order the change from one ventilator to another at any time. I knew a change was coming because my ventilator had been recalled and was still not repaired. Additionally, my respiratory DME (durable medical equipment) provider ended their contracted maintenance for that brand of respiratory equipment. My Respiratory Therapist (RT) and I had formulated a plan for me to transition to another ventilator (vent) brand when my unit would need its 10,000-hour regular maintenance near the start of 2024. At my neuromuscular pulmonary appointment in June 2022, I was advised I would no longer see the MD but would move to the Nurse Practitioner (NP) for subsequent appointments, as long as I remained stable. I saw that NP in June 2023, and changing vents was not part of our discussion. One month later, I was notified via the patient portal that this NP had sent an order for me to get a new vent. 2. Existing ventilator settings could be forgotten or even “up for debate.” My respiratory DME originally received the order for a new vent, but it was missing the settings to be enabled for my two prescriptions, (AVAPS AE for sleep and mouthpiece ventilation, as needed for daytime use). The settings were needed before delivery could be scheduled, so I sent a patient portal message to request those in a revised order. What happened next was unexpected, frightening, and infuriating. I had been on a tidal volume, the amount of air that moves into and out of the lungs in a cycle, of 525 ml for AVAPS AE mode for the last 5-6 years, and the order for the new vent specified 350 ml. My RT believed this reduction could be harmful to me. I was diplomatic but firm in my next patient portal message, explaining to my MD that the NP had ordered this reduction in tidal volume and I would refuse to use the new vent, as it was lower than what was prescribed in 2015. Further, I explained my medical records with this same medical practice show I’ve been using 525 ml for more than 5 years. Within hours, I received a response that an error had been made (albeit not clear as to why) and the order would be corrected with my current tidal volume and re-faxed. Unfortunately, that is not what happened. Copies of the incorrect order continued to be sent to my respiratory care DME, or they received nothing after each confirmation that another order had been electronically faxed. Phone calls between my RT and the nurse and NP occurred, and I continued sending periodic messages via the patient portal. By the time the RT received the corrected order, weeks had passed, and more than 20 messages had been sent back and forth about this vent. My RT believed the individuals involved in preparing the order were unfamiliar with IVAPS (Intelligent Volume Assured Pressure Support), the type of noninvasive ventilation I was moving to on the new vent, the near equivalent of what I was using on my existing vent, AVAPS (Average Volume Assured Pressure Support). The only plausible explanation he could think of for their initial tidal volume reduction was based on their knowledge of what tidal volume a person my size would need while intubated (receiving ventilation through an endotracheal tube), not considering noninvasive ventilation at home with an intentional leak and thus a necessary higher tidal volume. Whatever the reason, in the beginning of the process, I felt as though I had to fight to defend what had been keeping me stable for so many years, but my next source of anxiety was trying the new vent. 3. Your RT may have little to no experience with Neuromuscular breathing weakness ventilator settings. My RT lacks experience with neuromuscular noninvasive vent settings but makes up for that with his lack of ego, desire to continue learning, and respect for patients who have knowledge about their respiratory health. For that, I’m grateful. He was at my home multiple times and had no problem leaving my existing ventilator for use as I was adjusting to the new one. Vent settings orders often include a range of values with some degree of leeway for the RT to adjust for comfort. On vent delivery day, I made the mistake of not reclining (and I know better!) while trying the vent and later realized what felt okay while seated was intolerable while lying down. The breath triggering, length of time for each breath, and cycling in and out of inspiratory and expiratory pressures on the new vent were completely different from my old vent. I had moments that night while awake in bed that felt like I was struggling to get enough air. What would have happened if I had gone to sleep?! Having my old vent was critical to getting me through that first night and while waiting a couple of days until my RT could return to make adjustments to the settings. We had agreed up front that I would keep the old ventilator for at least a couple of weeks during this transition. 4. It may not be possible to use the same settings on the new ventilator. My old ventilator’s proprietary AVAPS mode had fields that do not exist in the new vent's IVAPS mode and vice versa. The same can be said about each vent's mouthpiece ventilation mode. Each manufacturer names settings differently, and units of measure (seconds versus milliseconds, liters versus milliliters, etc.) may also be different. This made it impossible to use the same settings in this transition. My RT had to provide a template of sorts for the clinician to use in revising their order so that all appropriate aspects of the prescribed settings were included. Ultimately, he had to get on a couple of phone calls to review the various settings with my pulmonary NP's RN. 5. The new ventilator may feel different from your previous ventilator. On my old vent, I used a 4.0 l/min flow trigger sensitivity, but I require what is labeled as very high triggering on the new vent. I required a flow cycle sensitivity of 20% on the old but 30% for the cycle setting to feel comfortable on the new. It was surprising to me that two manufacturers would have vents that are so different. This is why so many adjustments needed to be made after the initial vent setup provided on delivery day. I asked members of the Breathe with MD Support Group whether or not they had tried to transition from one manufacturer’s ventilator (used noninvasively or invasively) and had been unable to successfully do so. (This was during a time when I questioned if I would be able to successfully use the new vent.) I learned that no two vents, not even of the same model feel the same. One group member shared, “…even when my Trilogy vents get switched out for newer Trilogy (ie, when I reach the maximum blower hours), it still takes a day or two to adjust. Every vent is different even if it’s the same model. At least, that’s been my experience.” She continued, “If you think practically, it’s a machine and it’s virtually impossible for them to be identical. Unless I’m having major issues with a switch out, I give my body a few days to adjust to the new vent before I make any adjustments.” Another group member shared, “You'd expect two machines bought on the same day to perform the same but if not, one has more/less wear on seals, rings, and other parts to change pressures slightly.” 6. Multiple adjustments may need to be made to the new vent's settings. On his second visit, my RT got the new vent settings to feel closer to that of my old vent. It was tolerable for an entire night of sleep, but I was waking up due to an odd cycling difference. My RT has known me for several years and agreed that I could continue to try various minor setting changes on my own, something I was comfortable with and knew how to do. He had recommendations for things I could try, and I made note of them. 7. It takes time to adjust to the changes. After trying the new vent before having the updated and more tolerable settings, the muscles between my ribs felt a little sore each morning for the first few hours of the day. The longer I used the new vent, the more I realized it required more humidification than the old one to keep me from waking up with a very dry mouth. I had to try various temperature increases to finally arrive at the decision that an increase of 1.5-2 points was necessary. By the time I worked that out, the dryness triggered over-production of mucus (something I experience if I sleep without the humidifier on by accident), and I dealt with excess secretions for three to four days during my mechanical cough assistance therapy. I spent time reading about each setting on both the old and new vents to better understand them. This allowed me to more confidently make changes to the settings and arrive at comfort-type settings that made the new vent feel much closer in breath delivery to the old vent. It was an amazing feeling to achieve that, but I had to ensure my RT agreed with the changes. Thankfully, he was in agreement! If I had not made those changes on my own, the number of visits from my RT would have increased as would the duration of my sleep deprivation. And working, volunteering, and living with a Neuromuscular Disease (NMD) make lack of quality sleep extremely difficult for me. I had taken a full week off work for this vent transition, but delays in receiving the vent sadly meant most of those days were wasted. NMD Patients Changing Their Own Vent Settings? Now that I've shared those lessons, you may be wondering how common (or not) it is for an NMD patient to change their own vent settings. In the US, this happens more often than prescribing clinicians likely realize. I posted a poll in the Breathe with MD Support Group, and the responses give you an idea of how many are lacking needed NMD settings-knowledgeable RTs to support ventilator use and transitions like mine. I believe we have a problem that is rooted in a lack of NMD-specific curriculum content for RTs in training. Our being a minority in their caseload full of COPD (Chronic Obstructive Pulmonary Disease) and OSA (Obstructive Sleep Apnea) patients who are nothing like us only amplifies this.
Are their respiratory DMEs that specialize in NMD care? Sure, those exist, but they are like rare unicorns hiding in obscure places. Too many individuals living with NMD and their families are being forced to self-advocate at every step towards getting the care they need which includes mechanical ventilation initiation and every phase of its use, including the process of moving from one brand of vent to another. Speaking up is critical for our survival; otherwise, we suffer, even die prematurely. More Lessons to Come? I don't consider my old-to-new vent transition fully complete. I anticipate more lessons to come, as my prescriber will be reviewing the settings selected for comfort and my usage data. Until then, I'm thankful for every night of good sleep on my new vent! It is my hope that others navigating this same process have a less challenging time than I did. |
AboutLiving Ventilated celebrates those in the NMD community who use assisted ventilation. Archives
August 2024
Categories |
Breathe with MD, Inc. is a U.S. registered 501(c)(3) nonprofit organization. Donations are tax deductible to the extent allowable by law.
Note: This website should not be used as a substitute for medical care. For medical care or advice, please seek the care of a clinician who specializes in the breathing issues of those with Neuromuscular Disease (NMD).
Web Hosting by Hostgator
Note: This website should not be used as a substitute for medical care. For medical care or advice, please seek the care of a clinician who specializes in the breathing issues of those with Neuromuscular Disease (NMD).
Web Hosting by Hostgator

 RSS Feed
RSS Feed